Navigating the Healthcare Payments Racetrack – Part 1
The typical journey to payer reimbursements and patient payments is fraught with speed bumps, detours and plenty of tolls that add expense and slow inbound revenue. For this reason, trade publications, organizations and many healthcare bloggers devote a great deal of time to the subject of “optimizing the revenue cycle.” While there is a lot of good information out there, often you need to piece it together across different sources in order to see the bigger picture. That is, until now.
Below is a depiction of that bigger picture along with four initiatives providers can engage to eliminate key speed bumps and make the journey to revenue quicker and smoother.
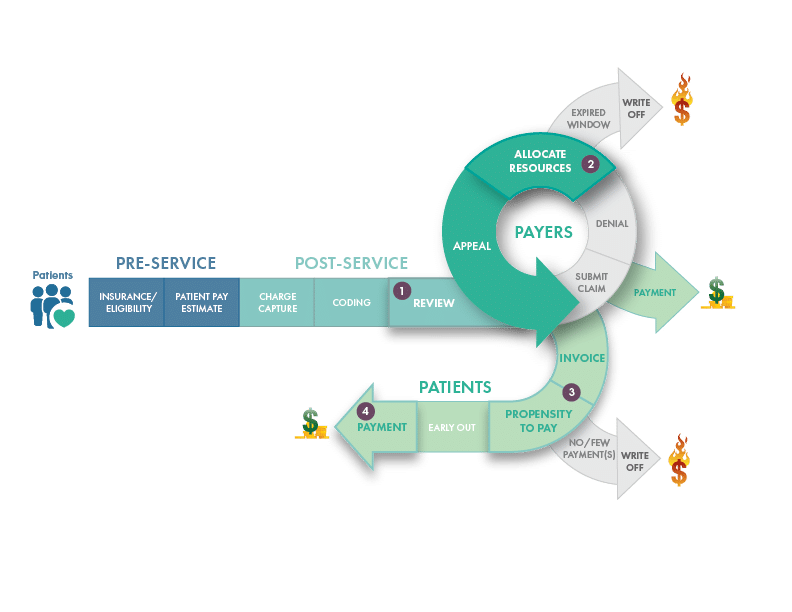
The following areas of the revenue cycle track often slow the flow of revenue:
- Review prior to submission of claim
- Allocate Resources to Appeal Denials
- Patient Invoicing / Propensity to Pay
- Patient Payments
We’ll review the initiative for each of these areas in greater detail over the next few posts. Let’s start with the speed bump that appears right before the claim is submitted.
Making Claim Reviews Smarter
The typical revenue cycle process often includes claim scrubbers and smart claim edits so that errors may be identified and corrected prior to claim submission. This approach is fine, albeit staff-intensive. However, since Payers are known to change the rules along the way, smart claim edits can become quickly outdated and cause the reimbursement process to take a detour straight to Denial-ville.
Denials are a problem, no doubt. It doesn’t matter if you’re a large healthcare organization or a small one, delays in reimbursements are costing these operations hundreds of millions in revenue. The best way to mitigate denials is to be just as dynamic with your claim edits as Payers can be with their rules. You do this by inserting loop learning into your process.
Loop Learning to Keep Pace with Payer Rule Changes
Loop learning is not about normalizing your data, although that is a necessary prerequisite. It’s about a continuous analysis of your data, specifically data found in your 837 and 835 files, so your claim edits can get smarter every day and adapt to the changes that payers often make. Staying on top of changes in payer requirements is particularly important to avoid clinical denials where the back and forth of additional information and medical records results in a significant slow-down in the process.
What You’ll Need for Loop Learning
While there is no lack of data in the healthcare industry, much of it exists in a not-easily-used format and resides in systems that don’t talk to each other. Your data hold valuable information that can help you reduce initial claim denials. But, to do that, you need a way bring that information together easily and link it correctly.
Actually, a data GPS system would be most helpful at mapping the path between your files — if such a thing existed. Unfortunately it does not so transforming your valuable, yet unusable data into workflow action means you’ll need access to a resource with tools and expertise to leverage your existing systems.
It doesn’t matter if you hire or partner for that expertise – you’ll need it. Sure, there’ll be an expense associated with acquiring those skills. But it may not be as hefty as you may expect – particularly when you think about the impact that thwarting even a small percentage of denials will have on your revenue flow.
Consider what a 5% swing in denials would do to your bottom line. How would that swing impact your 2020 KPIs? There’s a lot of revenue at stake. The quicker you get it, the better.
Next time in part two, we’ll be talking about getting rid of the next speed bump – appealing denials.



