…And Save Resources While You’re At It!
The journey from services rendered to reimbursement received can be extraordinarily slow if the initial claim has been denied by the payer. Think about the time value of money. Now think about all those claim dollars just parked in a rest area. That’s a lot of money earning a lot of interest for payers while your team burns through hours working on appeals so you can eventually get what is owed to you. That costs you big time – both in the slow travel of inbound revenue and the Autobahn speed of outbound payroll dollars.
Avoid This Mistake
Raise your hand if you prioritize appeals based on highest dollar value or on the age of the denial. If you’re like 90% of the providers I’ve talked to, your hand is in the air.
While either of these attributes seems like a logical place to start the appeals process, neither is as effective at securing timely revenue as providers would like. And, both tend to consume massive resource hours.
So ask yourself these two questions:
- “Am I happy with the return on my appealed denials?”
- “Am I happy with the amount of resources I allocate to working those denials?”
If you answered no to either question, it’s time for a change. Time to get off that old bumpy route and exit onto a superhighway that will not only yield greater claim dollars but will save you hours upon hours of resource time.
Know Which Denials Will Get Overturned
Your denial history is rich with learning that, if accessed and applied, can transform the way you appeal denied claims and the speed with which payer reimbursements flow back to your organization.
Your history will show you which denials will easily be overturned and which will never get overturned – regardless of dollar amount or age. If you don’t know what those denials look like, you’ll continue to expend resources on appeals that will yield no revenue for you – at least not any time soon.
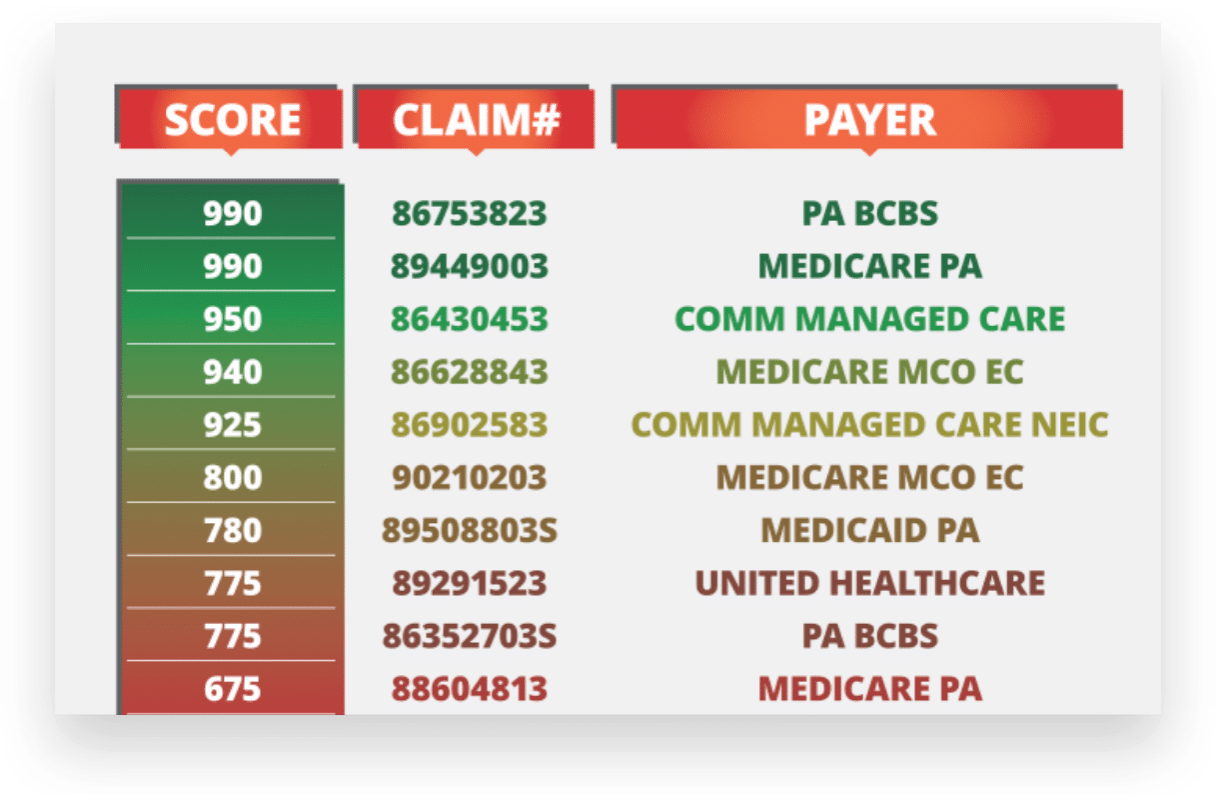
There are analytical and predictive tools available that can leverage your data to score and rank your denials in the order in which they are most likely to be overturned. Then, that ranking gets returned right back to your system and work queue for your staff to access. Sometimes those top rankings may include a high dollar denial or a denial that is getting close to its age limit. Other times they may be denials that are mid-level value and have just been denied. The point is knowing which denials to appeal first enables you to maximize your denial recovery while minimizing the resources you expend.
It’s kind of like the 80/20 rule. You can get 80% of denial recovery by working only 20% of the claims. The key lies in knowing which 20%.
Caution – Not all Models are Equal
Many vendors claim they can use models to help you, but be careful. Often they use only a handful of variables to build their models, when in fact hundreds of data variables should be used to ensure reliability. There is a lot of money at stake for your organization so don’t take short cuts with your predictive model.
If you have any questions or comments on which data to harness, how to harness it, or where to turn for predictive modeling, please let me know. I’m happy to point you in a direction that’s right for your facility.
Next time: How propensity to pay can revolutionize your patient payments!



